Cervical osteochondrosis is a progressive degenerative-dystrophic lesion of the intervertebral discs in the region of 1-7 vertebrae belonging to the cervical spine.
As a result of cervical osteochondrosis, deformations, exhaustion and thus damage to the vertebral bodies occur. This disrupts the normal blood supply and nerve conduction in the neck and in those areas that are innervated by the nerve roots of the cervical spine.
Cervical osteochondrosis can be isolated or combined with osteochondrosis of other parts: thoracic, lumbar and sacral.
causes
A number of factors are distinguished that predispose to the development of osteochondrosis. These include:
- sedentary and sedentary lifestyle;
- sedentary types of work with static load on the neck;
- overweight, insufficient physical development;
- dysplastic processes of connective tissue;
- circulatory disorders in the neck;
- neck injuries;
- scoliosis, poor posture, uncomfortable pillows and mattresses;
- hereditary predisposition, metabolic defects.
Cervical osteochondrosis symptoms. complications
The cervical spine is the most vulnerable to the development of osteochondrosis. The vertebrae contained in it are the smallest compared to other parts of the spine, the muscle structure is not very pronounced, the weight of the head and the upright posture act on the vertebrae. In the cervical spine, the vertebrae fit tightly to each other. Even the slightest change in them can lead to compression and even displacement of nerves and blood vessels.
The most characteristic symptom that patients complain about is pain in the cervical spine. Depending on the affected area, the pain can be localized: in the collarbone and shoulder; throughout the cervical spine; on the anterior surface of the thorax.
The first signs of cervical osteochondrosis can be insignificant: a feeling of heaviness in the head, headache in the occipital region, pain in the neck in the evening, a feeling of numbness or tingling in the shoulders and arms.
Main symptoms
Vegetative-dystonic.
Severe "stabbing" pain in the neck, in the area just below the occiput. Pain occurs after a long stay in one position, after sleep, constant tension of the neck muscles.
Difficulty moving the hand to the side, stiffness, numbness in the fingers. Due to the compression of the vertebral arteries, neurological manifestations are observed: headache, nausea, dizziness, unreasonable jumps in blood pressure.
Spinal symptom.
The pains are localized behind the breastbone on the left.
This type of pain should be distinguished from anginal pain (with angina pectoris, nitroglycerin brings relief, with osteochondrosis it does not).
With a gradual disruption of the structure of the intervertebral discs, they are compressed and violation of the nerve roots occurs, as well as narrowing or violation of the arteries and veins passing into the region of the vertebral bodies.
This leads to the formation of special syndromes - radicular and ischemic:
- defeat of the roots of the first cervical vertebra (C1): anomalies in the occiput;
- C2 lesion causes pain in the region of the crown and occiput;
- lesion of C3 gives neck pain from the side of the infringement, decreased sensitivity in the tongue and hypoglossal muscles, speech disorder is possible;
- damage to C4 and C5 causes pain in the shoulder and collarbone, decreased tone of the muscles of the head and neck, hiccups, respiratory distress and pain in the heart;
- C6 lesion occurs more often, gives pain from the neck to the shoulder blade, forearm, up to the thumbs, skin sensitivity can suffer;
- C7 lesion - similar symptoms with pain in the neck, back of the shoulder, up to the back of the hand, reduced arm strength and decreased reflexes.
Circulatory disorders due to the compression of blood vessels in the cervical vertebrae can lead to headaches, up to migraines, dizziness, visual disturbances and tinnitus, flashing flies in front of the eyes, disturbances of autonomic functions.
There may be manifestations of cardiac syndrome with pressing pain in the heart, lack of air and palpitations, rhythm disturbances.
Complications.
Protrusion of the intervertebral discs with the formation of a hernia (protrusion).
Rupture of the intervertebral disc with pinching of nerves and blood vessels, possible compression of the spinal cord, which can be fatal.
Root lesions (radiculopathy), formation of spines on the vertebral bodies (osteophytes) with the manifestation of paresis and paralysis.
In the presence of the above complaints, it is necessary to contact an orthopedist or neurologist and conduct the necessary research.
Nutrition
Proper nutrition will significantly alleviate the condition with osteochondrosis. Nutrition should be complete. If a person has a normal body weight, as a basis, you can take a therapeutic diet number 15 according to Pevzner. Contains all the necessary minerals and an increased amount of water-soluble fats and vitamins. It is necessary to eat foods rich in natural chondroprotectors. Chondroitin is found in goldfish, in animal tendons and cartilage, and in chicken meat.
Be sure to take clean water in a volume of 1. 5-2 liters. Fluid is needed to prevent the intervertebral discs from drying out.
Traditional and non-traditional treatments
Treatment
Today, there are traditional and non-traditional methods of treating osteochondrosis in the cervical spine.
Methods of drug treatment: symptomatic therapy with analgesics to relieve pain; taking non-steroidal anti-inflammatory drugs to relieve inflammation and tissue edema; antispasmodics; drugs to improve blood circulation; chondroprotector to restore the structure of the intervertebral discs.
A course of group therapy with vitamin B is shown, external agents for therapy - gels and ointments, creams with anti-inflammatory, warming and analgesic components.
During the period of exacerbation, it is recommended to wear a special collar (Shants collar).
Complications of cervical osteochondrosis with intervertebral hernias that impair sensitivity and blood circulation can be treated promptly.
The duration of treatment depends on the abandonment of the condition, since osteochondrosis is a chronic progressive disease. Treatment can be long, and preventive courses can be carried out throughout life.
Physiotherapy treatments.
These include physical therapy, magnetotherapy, balneotherapy, laser therapy, acupuncture, Lyapko's application therapy, and massage.
Physiotherapy
It is imperative to perform exercises for the treatment of cervical osteochondrosis several times a day every day. They include self-stretching, self-massage, a set of special exercises. Avoid neck injuries and heavy lifting.
It is necessary to combine prolonged sitting with periods of rest and warm-up.
At the base of the health of the cervical spine there is a strong and healthy back, physical activity, a comfortable bed with anatomic pillows and mattress, correct posture and proper nutrition.
Lyapko application therapy
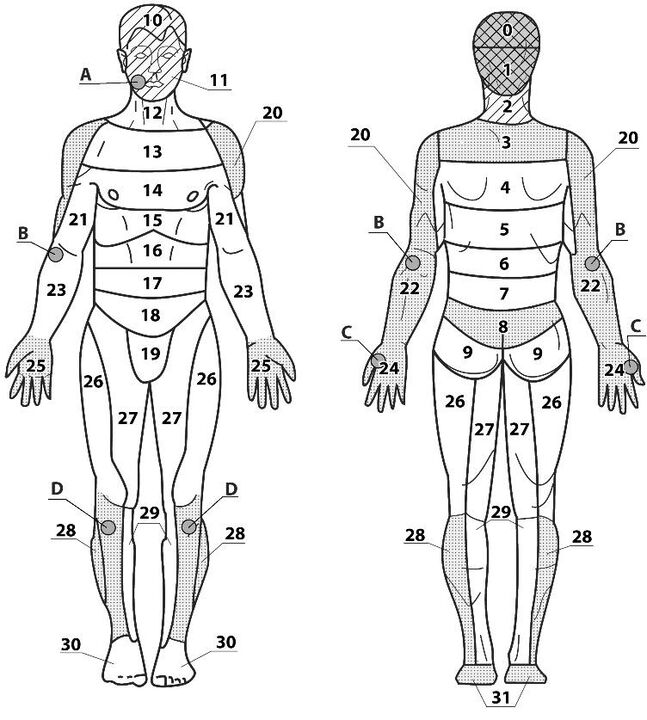
Areas of application:
- base 2, 3;
- further 1, 4, 12, 13;
- auxiliaries 20, 22, 28, 31.
General recommendations
When using the applicator, the main, additional and most painful areas are used, but in case of very pronounced pain, the applicators should be applied above and below the painful area, or points and areas on the opposite side should be used. Exposure time 10-30 minutes.

If cervical osteochondrosis is combined with osteochondrosis of other parts - thoracic, lumbar and sacral, then application therapy can be applied simultaneously or in turn to all parts of the spine. The larger the exposure area, the better the effect.
















































